
In recent years, as interest in nanosecond lasers has waned due to the rise of picosecond lasers, there has been a renewed movement to reevaluate the usefulness of Q-switched lasers. In this webinar, Dr. Kimura, who has extensive clinical experience in treating pigmented lesions, will comprehensively explain the basic principles of the Q-switched laser “TRI-BEAM PREMIUM,” treatment strategies for specific lesions, and the latest approaches, under the title “Rediscovering Q-Switched Lasers.”
- INDEX
Fundamentals of Q-Switched Lasers and Disease Characteristics (00:38-)

Q-switched lasers have been used to treat pigmented lesions such as solar lentigines, seborrheic keratoses, freckles, ADM, Nevus of Ota, and traumatic tattoos. Treatment requires full understanding of wavelength, absorption curves, and thermal relaxation time (TRT). For melanin, wavelengths (e.g., 532nm, 694nm, 755nm, 1064nm) are selected based on lesion depth (superficial or deep). Further, irradiation with a pulse width shorter than the target’s TRT enables selective destruction without damaging surrounding tissue.
Insured/Non-Insured Treatment(4:20-)

Q-switched laser treatment for pediatric birthmarks is often covered by insurance and can be applied to Nevus of Ota, Mongolian spots, and traumatic tattoos. Ruby laser treatment is covered for up to 5 sessions, and flat birthmarks are covered for up to 2 sessions. Self-pay treatments at our hospital primarily include solar lentigines, freckles, and ADM. For solar lentigines, IWP, scabs, or PIH may occur after laser treatment, but these improve with appropriate laser application and follow-up observation. Even when ADM does not improve with IPL, ruby laser treatment can be effective in some cases; selecting the appropriate wavelength based on lesion depth is crucial.
Current Understanding of Melasma Treatment and the Role of Lasers (11:54–)
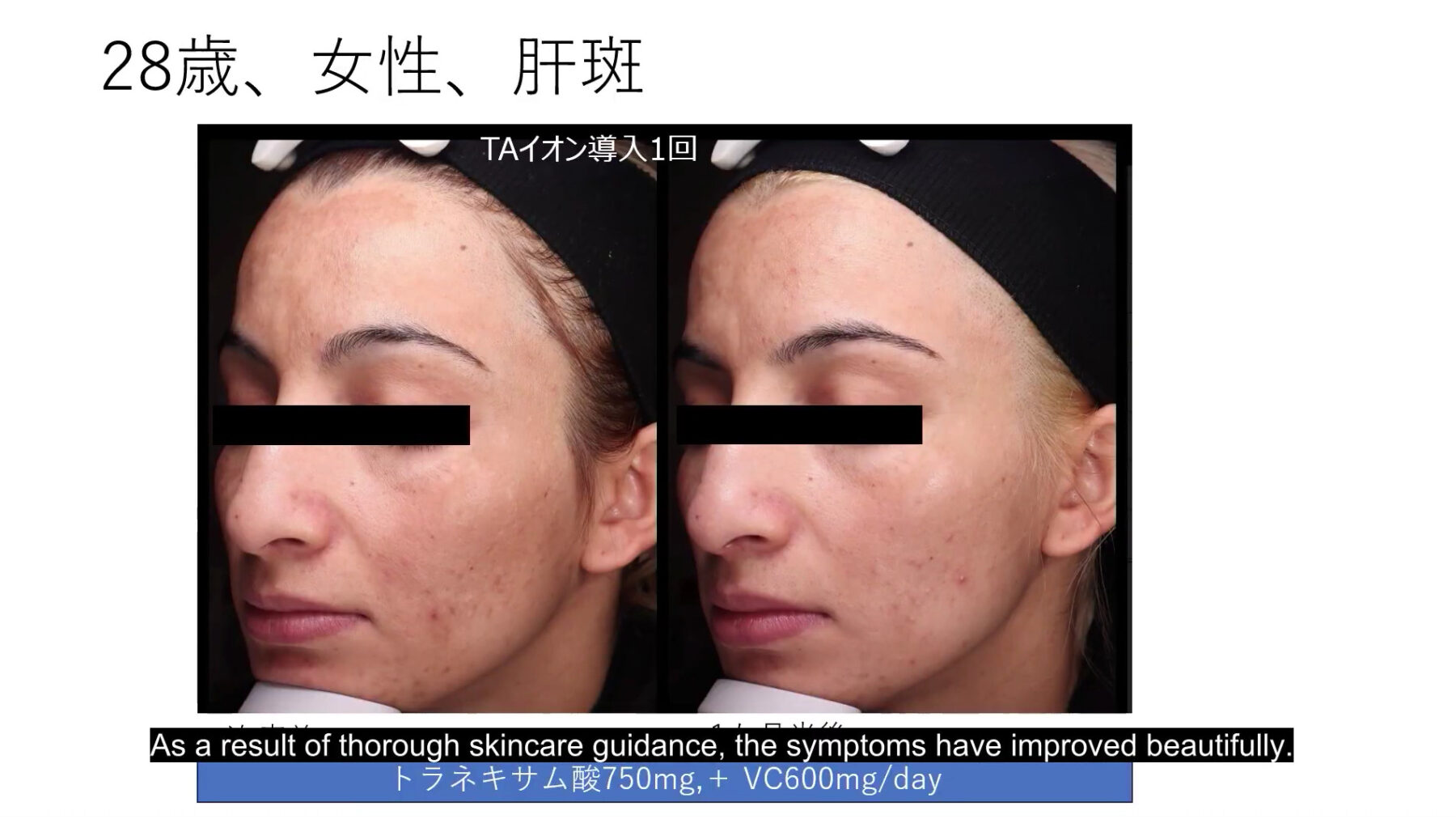
Melasma is commonly seen in Asian women in their 30s to 50s, with UV exposure, friction, and female hormones playing complex roles. The mainstream theory is that “abnormalities in the epidermis and dermis due to photoaging” activate melanocytes. Increases in α-MSH, VEGF, and prolactin receptors have also been reported. As impaired stratum corneum barrier function, basement membrane damage, and dermal vascular proliferation are deeply involved, primary treatment focuses on UV protection, avoiding friction, and moisturization. Tranexamic acid effectively suppresses cytokines and is commonly used with vitamin C. “Laser toning” using a 1064nm low-fluence laser is also an option. However, for melasma involving basement membrane damage, high-fluence lasers carry a risk of depigmentation, requiring utmost caution. Follow-up after toning is essential to prevent recurrence and depigmentation.
Practical Approach Utilizing TRI-BEAM PREMIUM (22:30–)

Finally, regarding Jeisys’s TRI-BEAM PREMIUM. Equipped with 532 nm and 1064 nm, it selectively utilizes True Top-Hat, Gaussian, and GN mode to address pigmentation, redness, and dermal treatments. GN mode, in particular, works as a long-pulse Nd:YAG laser, excels in treating redness and dermal remodeling. Its PTP function, reducing pain, also contributes to patient satisfaction. In practice, 532nm spot irradiation yields good results for solar lentigines and freckles, while 1064nm True Top-Hat mode is effective for ADM. For melasma cases, an effective approach involves first using GN mode to improve redness and remodel the dermis, followed by Q-switched 1064 nm toning. It achieves results by treating three targets—melanin, the basement membrane, and the dermis—in stages. GN mode is also effective for redness in rosacea-associated cases. A major advantage of TRI-BEAM is its ability to execute multiple treatment strategies with a single device.



