Yoko Yoshioka, M.D.
Director, Takanashi Clinic
Introduction
Edge ONE is a state-of-the-art carbon dioxide (CO2) laser. It is associated with less pain during irradiation and reduces post-treatment downtime compared to conventional devices. This device has a unique pulse mode that minimizes thermal damage to surrounding tissue, vaporizing only the tissue at the treatment site. The benefits to patients include fewer side effects due to less damage to normal tissue. In this article, through our experience of use and case reports, the effectiveness of Edge ONE as a minimally invasive and highly satisfactory treatment method is reported.
1 Basic Principles of Edge ONE
Principles and features of Edge ONE
Edge ONE, a medical device, is a gas laser with a wavelength of 10.6 µm (in the infrared range). The active laser medium is mixture of 3 gases consisting of carbon dioxide, nitrogen, and helium. This laser works on the basic principle of oscillation by excitation and resonance caused by electrical discharge.
Lasers are widely used in applications such as tissue cauterization because their wavelengths are readily absorbed by water, which is the major component of most human tissue. Edge ONE allows the laser light to reach slightly deeper skin layers, so that areas that are not vaporized form a thermal coagulation layer, thus also providing a hemostatic function. The laser exhibits excellent oscillation efficiency, facilitating irradiation at many different oscillation times (pulse widths). And the impact of light absorption by wavelength on water can be controlled by adjusting the irradiation time. The laser system also incorporates a fractional function, making it a laser device that incorporates all the fundamental elements of aesthetic therapy.
Edge ONE Surgical mode
The Edge ONE Surgical mode has four key features (Figure 1), the most important of which are the high power of 30 W and the ULTRA mode. These two features have a significant impact on reducing post-operative downtime, and the presence or absence of post-inflammatory hyperpigmentation (PIH) and scarring. Another feature of this mode is the inclusion of laser idling technology. This is a laser with a steep rise that does not apply additional heat to the surrounding tissue. The laser is very sharp and provides a good field of view due to low carbonization, making it useful for complex procedures. Additionally, the device incorporates five irradiation modes, allowing physicians to adapt treatment to different cases. The continuous wave (CW) mode emits laser light at a constant intensity while the switch is on. This mode allows physicians to perform dissection and coagulation using a technique similar to that of an electro cautery knife. Due to the significant thermal damage, it has a high hemostatic effect, which helps in hemostasis. In contrast to the CW mode, the ULTRA mode allows the pulse width to be narrowed to minimize thermal damage to surrounding tissue. This mode provides a better field of view due to less charring. In particular, when treating flat moles, Clark’s nevus and milia of 5 mm or less, the downtime is much shorter, increasing patient satisfaction. Indications for the surgical mode include moles, seborrheic keratosis, senile warts, acrochordon, flexible fibroma, warts, syringoma, xanthoma, condyloma acuminatum, milia, senile hemangioma (cherry spot), drainage of active acne, atheroma, and skin tags.
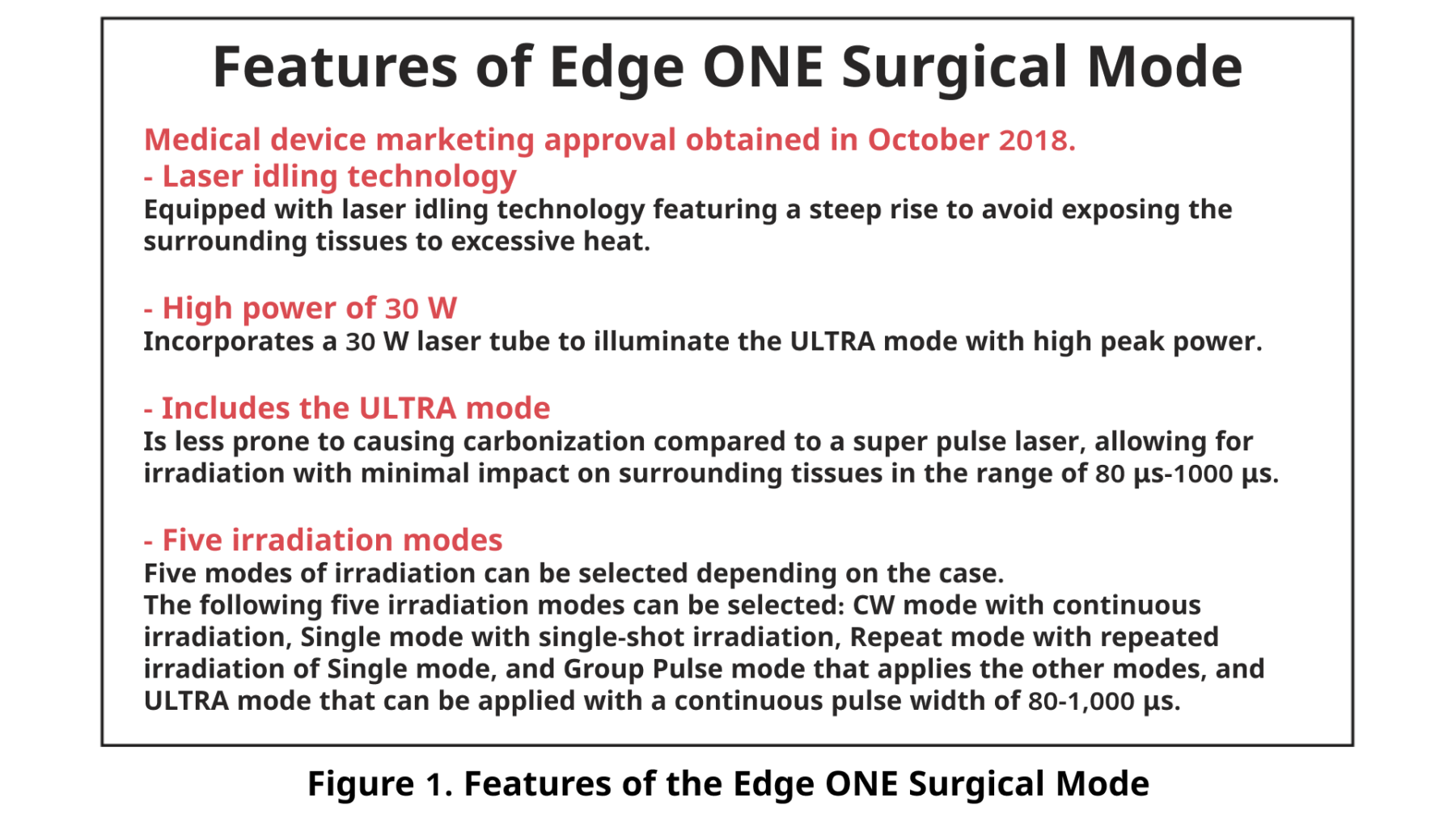
Figure 1. Features of the Edge ONE Surgical Mode
2 Examples of Treatment with Edge ONE (Surgical Mode)
Principles and features of Edge ONE
Figure 2 shows a case of a raised mole with a diameter of 5 mm. In this case, as an example of moving from the incision mode to the ablation mode, an approach was taken from the tumor side in the incision mode and the elevated part was resected. The ULTRA mode was then used to vaporize residual dye and trim the surface. Concentrating heat on one area of the skin can increase the risk of thermal damage, resulting in prolonged downtime; it is therefore important to perform the procedure quickly without stopping after excision.
Figure 3 shows a case of a raised mole. In this case, the CW mode was used followed by the ablation mode. First, the surface of the raised mole was flattened with the CW mode, and then the ULTRA mode was used; it is also important to move the hand quickly to avoid applying heat to a single point. Enlarging the excision area by about two sizes larger than the lesion helps reduce the likelihood of scarring. Especially in the area around the mouth or under the nose, where keloids are more likely to occur, a favorable outcome can be expected if this technique is adopted. The time required to remove two moles was approximately 3 minutes and 35 seconds.
Flat moles can be vaporized and removed using just the ULTRA mode. In the final step of mole removal, a dermascope is used to confirm the presence or absence of remaining tissue to complete the procedure.

Figure 2. Before and after mole procedure

Figure 3. Flattening raised moles
Key points for minimally invasive procedure
The first key point of minimally invasive treatment is the procedure technique. Gentle and prolonged treatment can cause extensive thermal damage to surrounding tissues, resulting in pigmentation, and possibly scarring. It is therefore important to reduce unnecessary thermal damage by repeating the cooling process while wiping the charred tissue with saline-soaked gauze, etc., after irradiating with the laser for about 5-10 seconds. The tip of the small diameter beam should be moved continuously to avoid irradiating the same area. This technique must be mastered because it significantly affects downtime and post-treatment outcomes.
The second key point of minimally invasive treatment is the puncture technique for local anesthesia. A local anesthetic should be injected after careful evaluation of the peripheral nerve course. This can help relieve the patient’s pain. When injecting an anesthetic into a mole, the needle should be inserted into the center of the sensory nerve tract in a proximal-to-central direction. This allows the physician to reduce the injection volume because the peripheral (distal) side has already been anesthetized. This may help reduce pain. When anesthetic is injected at multiple sites, an injection at the central region will provide anesthesia to the entire area; therefore, no pain may occur when the anesthetic is reinjected. When using the laser on forehead lesions, I perform a supraorbital nerve block (Figure 4). This nerve block can eliminate the need for multi-site anesthetic injections and reduce the risk of internal bleeding and pain.

Figure 4. Supraorbital nerve block
The third key point of the minimally invasive treatment involves shaving the surrounding normal tissue in a wide and gentle manner after complete removal of the lesion. This eliminates any elevation with the surrounding tissue and prevents concavity and scarring. In our clinic, closure therapy and moist wound care are implemented postoperatively. There is a risk of residual depression because the crusts epithelialize underneath. During follow-up visits, it is important to determine that hydration is being maintained. Preferably, the moist environment should be maintained for approximately 2 weeks.
The fourth key point of minimally invasive treatment is whether or not to use laser devices equipped with a scanner function. Many laser devices with a scanner have a mirror or computer that emits laser beams evenly and over a wide area. However, a type of scanner that illuminates the skin surface with a low-power continuous wave laser should be avoided because of the increased thermal damage to the hypodermis or subcutaneous tissue, which increases the risk of burns and scarring. Moreover, areas of varying thickness within the same lesion may not require the use of a scanner because of the need for additional radiation. While not categorically rejecting all devices with scanners, when considering the possibility of inducing post-inflammatory hyperpigmentation (PIH) after treating a wide area with a scanning laser, caution is required, and the treatment is considered risky.
The fifth key point of minimally invasive treatment (Figure 5) is the procedural difference between the punch excision technique and carbon dioxide (CO2) laser treatment. Punch excision is a technique in which a full-thickness lesion is excised with a skin biopsy punch and allowed to heal spontaneously without sutures. The advantages of this technique include ease of learning and less impact on surrounding healthy tissue. One of its disadvantages is that it creates a complete full-thickness defect after treatment. Such a defect undergoes a healing process of contraction of the wound and epithelialization from the surrounding tissue. On the other hand, CO2 laser treatment rarely causes a full-thickness defect even if the central part of the skin is slightly deepened. And because of the small amount of remaining dermis after treatment, the wound area undergoes little shrinkage. In other words, punch excision is a technique that actively creates a full-thickness defect to induce wound contraction. In contrast, CO2 laser treatment aims to retain the dermis as much as possible, avoiding flattening the surface and wound contraction. There is no absolute superiority or inferiority between the two techniques. However, I have not used the punch excision technique.
Figure 5: Difference between punch excision and CO2 laser
Diseases for which CO2 laser treatment is unsuitable
Those with findings suggestive of malignancy including malignant melanoma, lentigo maligna, and basal cell epithelioma.
Summary of Edge ONE Surgical mode (Figure 6)
The advantages include the high power output of 30 W, incorporation of ULTRA mode, short downtime, minimal post-operative side effects, and high patient satisfaction. The laser makes it possible for physicians who are accustomed to using CO2 lasers to achieve improved sharpness and have a comfortable user experience. The laser itself is also cost-effective with no need for consumables.
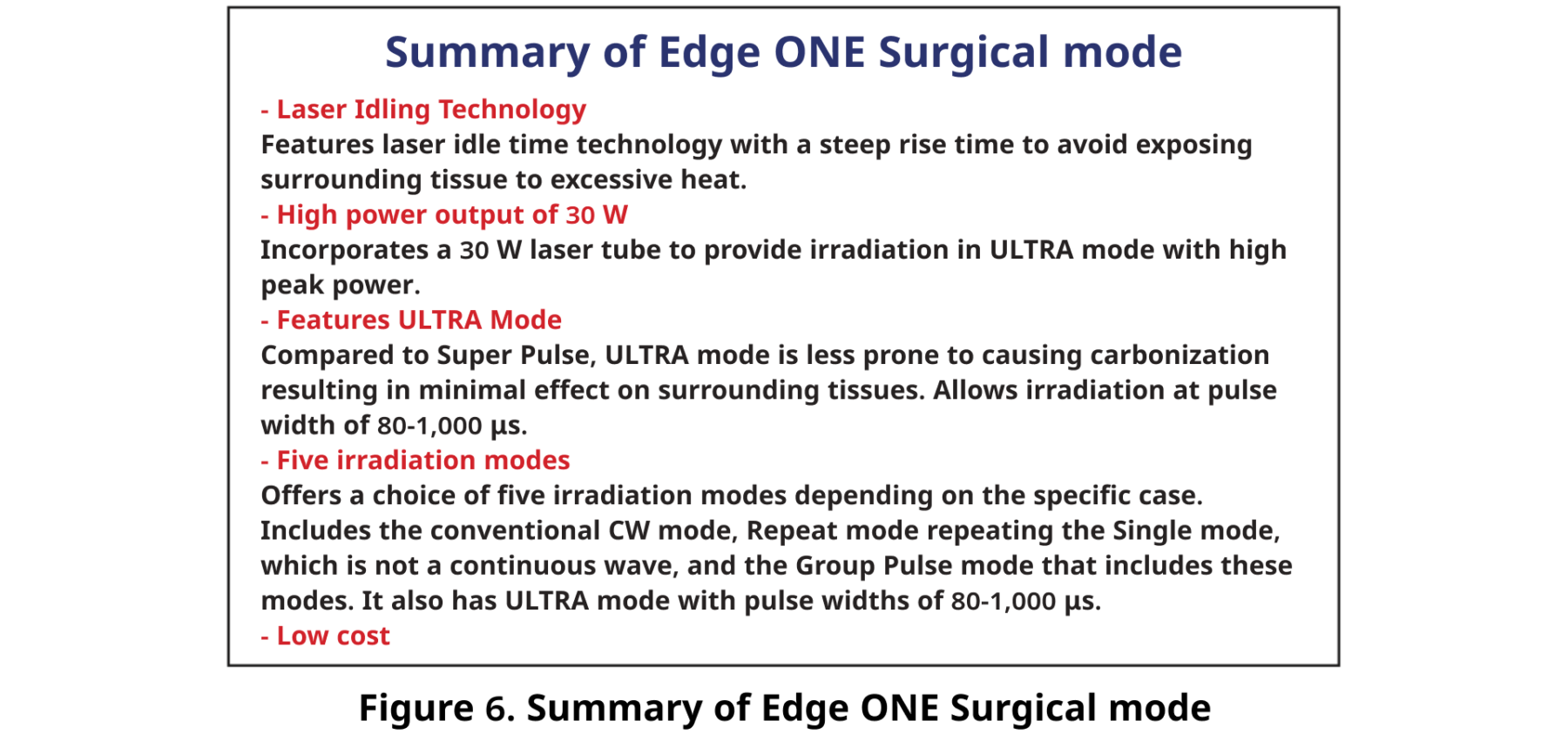
Figure 6. Summary of Edge ONE Surgical mode
3 Edge ONE Fractional Mode
Features of Edge ONE Fractional mode
The Edge ONE Fractional mode has the following features (Figure 7):
It incorporates three different scan shapes, taking into account the thermal relaxation time, and four beam patterns.
Stacking mode and moving mode, which provide deeper ablation, can prevent “missing spots” when only the stamping mode is used. Also, the five most commonly used parameters can be preset. The specifications are designed for ease of use by the operator because the scan size and scan pattern can be readily changed on the hand piece.
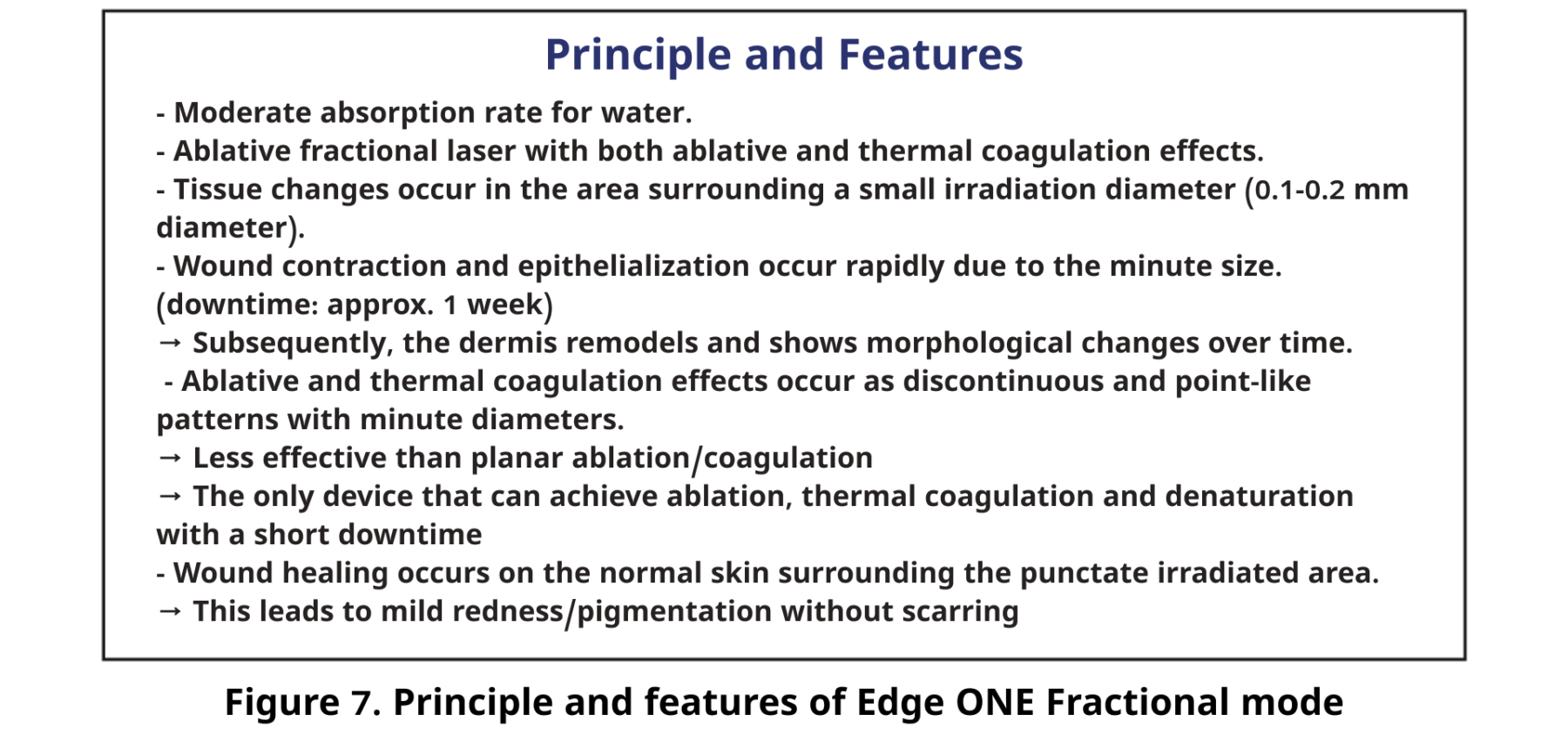
Figure 7. Principle and features of Edge ONE Fractional mode
The depth of penetration into tissue can be varied by changing the spot size (Figure 8).
The three scan shapes (Figure 9) can also be changed. In our clinic, the square and the triangular shapes are selected for flat cheek and nose areas, respectively. The four beam patterns include the Standard pattern for vertical irradiation, the Refresh pattern for reducing the appearance of post-irradiation spots and the Random pattern that slightly reduces downtime. Indications for the Fractional mode include skin rejuvenation, laser peeling, acne scarring, scarring, pore dilation, and wrinkling.

Figure 8: Various spot sizes

Figure 9. Scan shape and beam pattern
4 Edge ONE Treatment in Medical Settings (Fractional Mode)
Outcome of Fractional mode treatment
After topical anesthesia, irradiation treatment involves overlapping and two passes; one additional pass is added to the area that needs the most improvement. Mild redness and dotted or lattice-shaped irradiation marks are observed on the skin immediately after irradiation. The day after treatment, the redness disappears and the irradiation scars are no longer noticeable; makeup can be applied.
In the case shown in Figure 10, pigmented spots are being treated with a combination of tretinoin and hydroquinone, resulting in the entire skin being brightened. Figure 11 shows a case involving pores, showing significant improvements in sagging and blackheads.
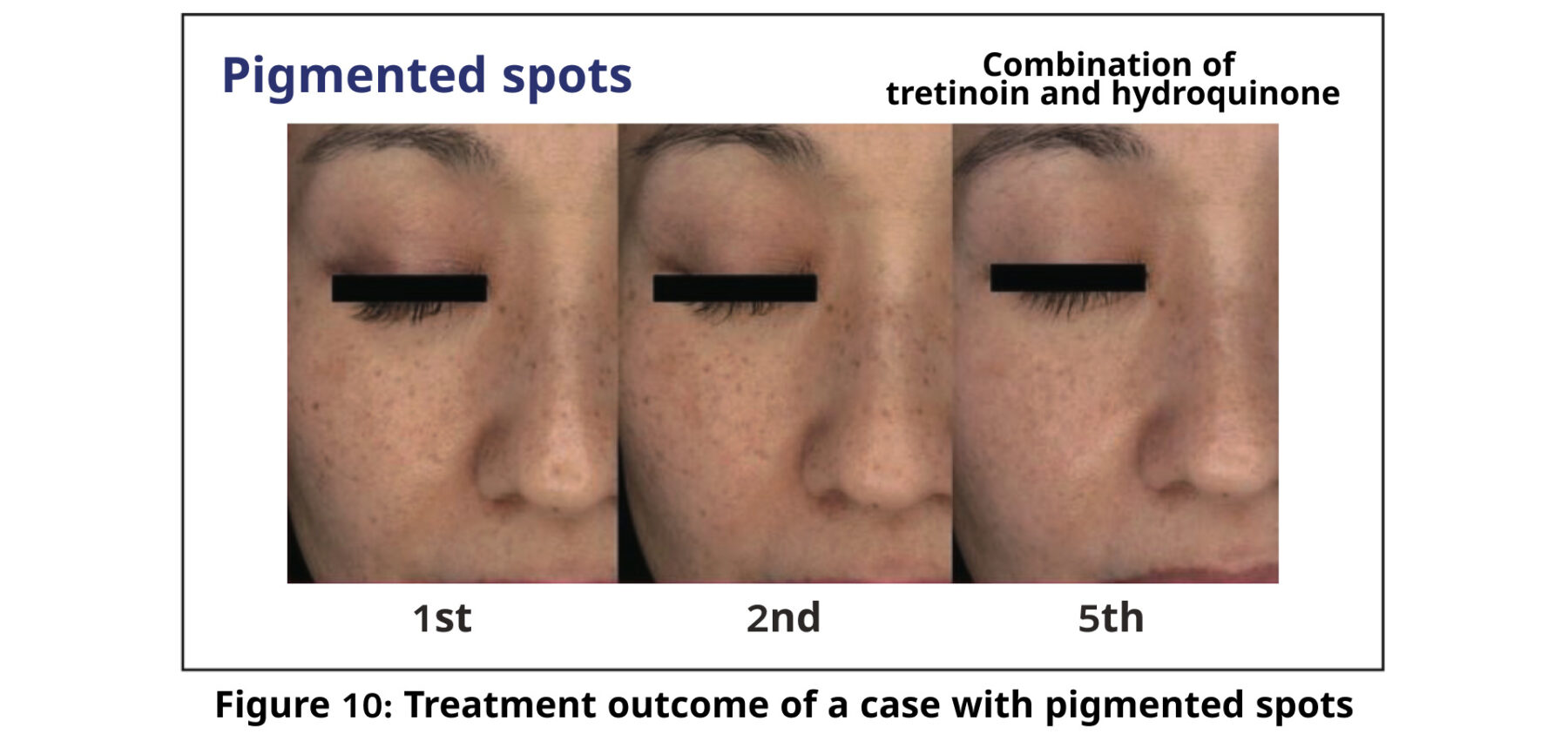
Figure 10: Treatment outcome of a case with pigmented spots

Figure 11: Treatment outcome in a case of hair pores
Key points of minimally invasive treatment
To conclude, in this section, I will discuss the optimal use of fractional lasers because many treatments for scarring have recently become available. Scarring caused by acne or a cut is a condition in which a certain proportion of scar tissue is distributed among normal skin tissue. Therefore, when fractional laser irradiation is applied to the entire surface, the burnt proportion of both normal skin tissue and scar tissue is the same, and the ratio of scar tissue to normal skin tissue cannot be reduced. For this reason, I believe that only the lesion area should be irradiated. Collagen fibers can proliferate and regenerate after irradiation, whereas elastic fibers and skin appendages do not regenerate. Based on actual cases, I believe that irradiation is effective for small scars only if the lesion area is irradiated.
Summary of Edge ONE Fractional Mode
The following summarizes the Edge ONE Fractional mode:
1: Three beam sizes
2: Three skin shapes and four beam patterns taking thermal relaxation time into account
3: Stacking mode for deeper vaporization
4: Equipped with moving mode
5: Preset for five parameters
6: Handpiece maneuverability
Hopefully, physicians will gain a thorough understanding of each characteristic of the device and apply them in their treatment.

